Depression is classified as a mood disorder. It may be described as feelings of sadness, loss, or anger that interfere with a person’s everyday activities.
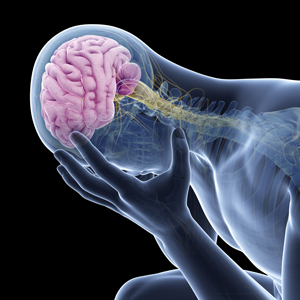
While depression can affect a person psychologically, it also has the potential to affect physical structures in the brain. These physical changes range from inflammation and oxygen restriction, to actual shrinking.
In short, depression can impact the central control center of your nervous system.
For those interested in learning more about how depression can affect the physical brain, and ways to potentially avoid these changes, we’ve laid it all out for you.
Brain shrinkage
The latest research shows that the size of specific brain regions can decrease in people who experience depression.
Researchers continue to debate which regions of the brain can shrink due to depression and by how much. But current studies have shown that the following parts of the brain can be affected:
- hippocampus
- thalamus
- amygdala
- frontal
- prefrontal cortices
The amount these areas shrink is linked to the severity and length the depressive episode lasts.
In the hippocampus, for example, noticeable changes can occur anywhere from 8 months to a year during a single bout of depression or multiple, shorter episodes.
That said, when a section of the brain shrinks, so do the functions associated with that particular section.
For instance, the prefrontal cortex and amygdala work together to control emotional responses and the recognition of emotional cues in other people. This can potentially contribute to a reduction in empathy in individuals who have postpartum depression (PPD).
Brain inflammation
There are also new links being made between inflammation and depression. It’s still not clear, however, whether inflammation causes depression or vice versa.
But brain inflammation during depression is linked to the amount of time a person has been depressed. One recent study showed that people depressed for more than 10 years showed 30 percent more inflammation compared to people depressed for less time.
As a result, significant brain inflammation is more likely to be relevant in persistent depressive disorder.
Because brain inflammation can cause the cells of the brain to die, this can lead to a number of complications, including:
- shrinkage (discussed above)
- decreased function of neurotransmitters
- reduced ability of the brain to change as the person ages (neuroplasticity)
Together these can lead to dysfunctions in:
- brain development
- learning
- memory
- mood
Oxygen restriction
Depression has been linked to reduced oxygen in the body. These changes may be due to changes in breathing caused by depression — but which comes first and causes the other remains unknown.
A cellular factor produced in response to the brain not getting enough oxygen (hypoxia) is elevated in specific immune cells found in people with major depressive disorder and bipolar disorder.
Overall, the brain is highly sensitive to reductions in oxygen, which can lead to:
- inflammation
- brain cell injury
- brain cell death
As we’ve learned, inflammation and cell death can lead to a host of symptoms associated with development, learning, memory, and mood. Even short-term hypoxia can lead to confusion, much like what’s observed with high altitude hikers.




























No comments:
Post a Comment